Introduction to Digital Diabetes Management
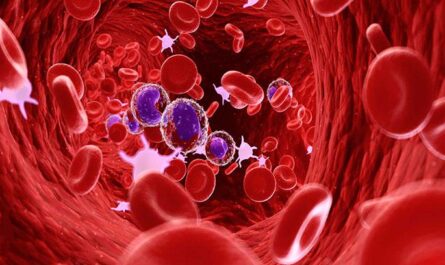
Diabetes is a chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. Insulin is a hormone that regulates blood sugar. Hyperglycemia, or raised blood sugar, is a common effect of uncontrolled diabetes and over time leads to serious damage to many of the body’s systems, especially the nerves and blood vessels. The most common forms of diabetes are type 1 and type 2 diabetes. Type 1 diabetes occurs when the immune system attacks and destroys the beta cells in the pancreas that produce insulin. Type 2 diabetes occurs when the body develops a resistance to insulin and/or does not produce enough insulin to maintain normal glucose levels.
Adoption of Digital Tools
The management of diabetes continues to evolve with advancements in technology and digital health solutions. More people with diabetes are adopting digital tools to help track blood sugar levels, carbohydrate intake, medication dosages and other factors that impact blood glucose. Devices like continuous glucose monitors (CGM), health apps, remote monitoring solutions, and automated insulin delivery systems are providing new ways for people to manage their condition. However, the successful adoption and optimal use of these technologies relies on several factors.
Continuous Glucose Monitors (CGM)
One of the most significant Digital Diabetes Management advances is the development of continuous glucose monitors which allow users to continuously monitor their glucose levels. Traditional fingerstick tests only provide a single blood glucose reading at a specific point in time, but CGM devices use a small sensor inserted under the skin to measure glucose levels in interstitial fluid every few minutes. This frequent glucose data in real-time helps diabetes patients and clinicians better understand patterns and tendencies. It enables timely treatment responses to avoid dangerous highs and lows. Many CGM systems can now alert users when glucose levels pass certain thresholds. They also eliminate the need for routine fingerpricks and provide a clearer picture of how various activities impact blood sugar.
Health Apps
There are thousands of diabetes apps available to support self-management. Apps enable logging of food, activity, medications, and glucose readings. They analyze entered data to identify patterns and provide insights about how to improve control. Many apps sync directly with blood glucose meters and CGM devices for automatic data uploads. This reduces manual data entry and human error. Apps also offer educational diabetes content, meal planning tools, reminder functions and connectivity with other users for support. Interactive apps with gamification features have shown potential to increase engagement especially in youth with diabetes. Telehealth platforms incorporating remote monitoring capabilities via connected devices and apps are growing.
Automated Insulin Delivery Systems
Research into artificial pancreas or closed loop systems is rapidly progressing. These combine CGM with automatic insulin delivery via insulin pumps. When glucose levels rise, the system automatically increases insulin delivery without user input. This differs from traditional insulin pumps which require users to manually administer insulin based on readings. The first hybrid closed loop system was approved by the FDA in 2016 and fully automated closed loop systems are expected to reach the market soon. Fully automated systems hold promise to significantly reduce burden of intensive insulin management and improve outcomes especially for those struggling with glycemic control.
Barriers to Optimal Usage
While digital solutions can revolutionize diabetes care, optimal adoption and consistent use remains challenging. Key barriers include: lack of insurance coverage or affordability, discomfort with new technologies, digital illiteracy in some groups, reluctance to relinquish self-management control, and usability issues with complexity of some solutions. Clinical studies also indicate significant drop-off rates in continued active usage of digital tools over the long-term. Busy lifestyles and ‘digital fatigue’ also impact sustained engagement. Uncertainty around data security and privacy risks are additional concerns especially for health data sharing. Overcoming these barriers requires education, usable designs, culturally-sensitive programs and involvement of care teams.
Digital Therapeutics and Coaching Support
Digital therapeutics which can deliver clinically validated therapeutic interventions via apps and digital platforms are emerging. These focus on behavior change techniques to better support chronic condition management. Coaching programs integrated within digital solutions also provide expertise, accountability and individualized guidance. Remote monitoring and data sharing enable clinical oversight without frequent visits. Outcomes studies demonstrate improved glycemic control particularly when digital tools are combined with coaching and behavior change strategies versus just reliance on self-directed usage. Social support from online communities can enhance engagement and empowerment. Successful diabetes digital therapeutics will be those providing personalized, evidence-based and sustainable support.
Impact on Healthcare Systems
Widespread adoption of proactive digital diabetes management through CGM, insulin pumps, health apps could transform the delivery of diabetes care. Greater insight into real-time glucose patterns enables timely treatment changes and avoids serious complications over the long run. This has the potential to significantly reduce healthcare costs of diabetes which stands at $327 billion annually in the US alone according to the American Diabetes Association. Remote monitoring through digital platforms could reduce need for frequent in-person visits especially for those with well-controlled diabetes. Data sharing may help identify patterns to predict and prevent adverse events much earlier. With integration, digital solutions could automate disease registries, treatment plans, medication management and quality improvement initiatives. Optimal digital diabetes management can help bend the cost curve while improving quality of life.
Advancements in digital health have augmented traditional diabetes treatment approaches. In the immediate future, automated insulin delivery systems combined with digital therapies and remote monitoring could revolutionize diabetes management. However, overcoming barriers to consistent use such as usability, affordability and lack of clinical integration will determine whether digital tools achieve their full potential or become just another abandonware. Success will require collaboration between technology companies, healthcare providers, payers and patients to enable sustainable behavioral and clinical support. With continued innovation and focus on human-centered design, digital health has immense potential to transform how diabetes is managed worldwide.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163)