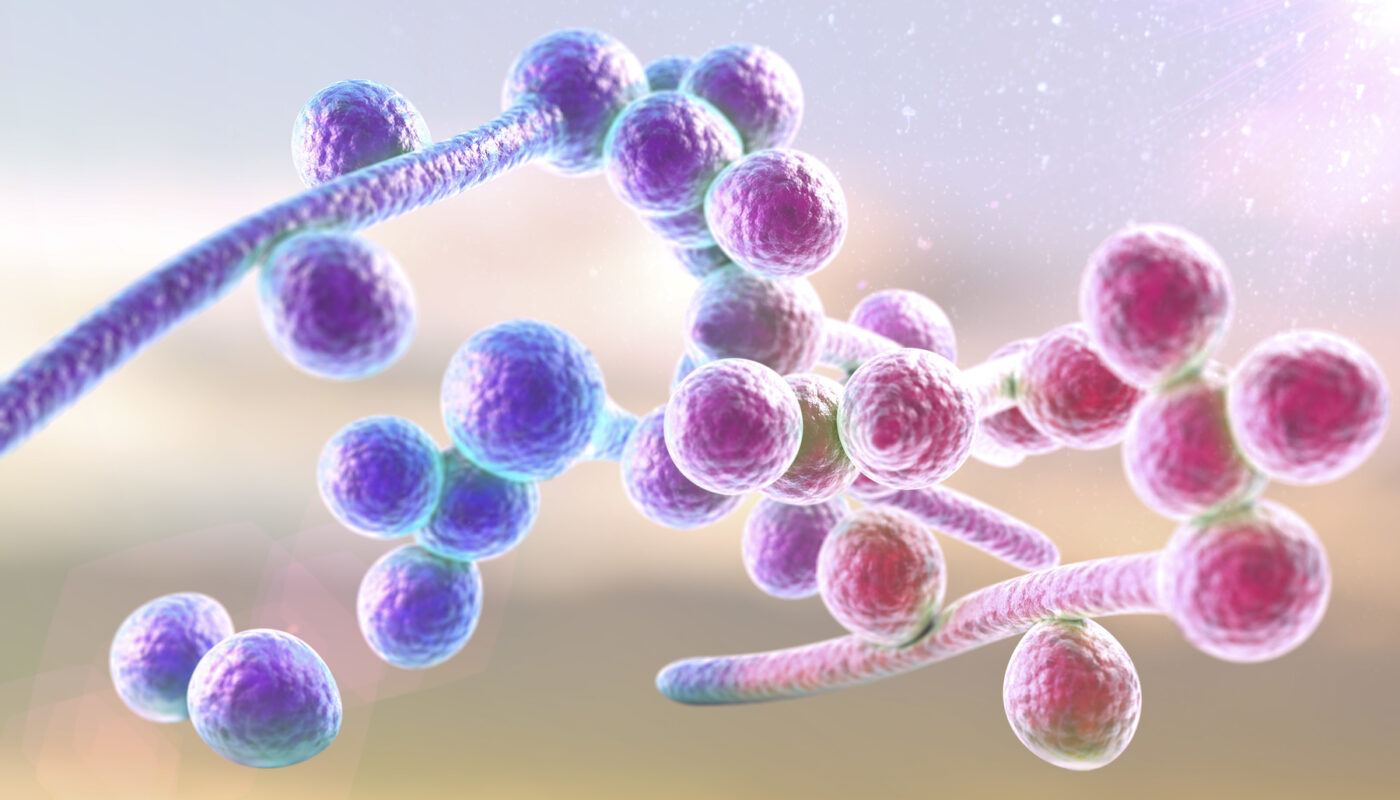
Candidiasis is a fungal infection caused by any type of Candida, a type of yeast (a fungus). There are over 20 species of Candida that can cause infection in humans. Candida albicans is the most common cause of candidiasis. The infection has different names depending on where in the body it occurs. Candidiasis can range in severity from superficial, minor infections to life-threatening systemic infections.
What are the common types of Candidiasis?
Oral Candidiasis (Thrush)
Candida infections of the mouth are commonly called oral thrush or oropharyngeal candidiasis. It is one of the most common fungal infections in humans. Thrush appears as white or yellowish patches that can form on the tongue or inner cheeks. These patches are actually clusters of Candida which proliferate in the warm, moist areas of the mouth. Oral thrush can occur in babies, denture wearers, people taking antibiotics, or those with weakened immune systems.
Vulvovaginal Candidiasis (Yeast Infection)
Vulvovaginal Candidiasis refers to Candida infection of the female genital tract, specifically the vulva and vagina. It commonly presents as thick, white vaginal discharge and vulvar itching or soreness. Vulvovaginal candidiasis is very common, with up to three-quarters of all women experiencing at least one episode during their lifetime. Predisposing conditions include pregnancy, hormone therapy, uncontrolled diabetes, and use of antibiotics.
What causes Candidiasis?
Candida organisms are normally present in small quantities in the mouth, intestinal tract and vagina. However, overgrowth of Candida can occur when the natural defenses against Candida are compromised or the balance of microorganisms is altered. This allows the fungus to proliferate and cause an infection.
Some common risk factors that can predispose to Candida overgrowth include:
– Use of antibiotics: Broad-spectrum antibiotics can kill protective bacteria and promote yeast overgrowth.
– High-sugar diets: Yeasts thrive on glucose, so high-sugar diets may facilitate Candida proliferation.
– Hormonal changes: Conditions like pregnancy with fluctuating hormones can increase the risk of a vaginal yeast infection.
– Immune suppression: Diseases like HIV/AIDS, cancer treatments and long-term steroids impair the ability to fight fungal infections.
– Medical devices: Intravenous lines, urinary catheters, dentures and other prosthetics can allow Candida access to tissues.
– Underlying diseases: Medical conditions like diabetes, autoimmune diseases and genetic disorders predispose to candidiasis through physiological changes.
Treatment Options for Candidiasis
For most Candida infections, antifungal medications are effective treatments. The specific therapy depends on the type and site of infection as well as any underlying health conditions.
Oral thrush is commonly treated with antifungal medication in the form of troches, lozenges or oral suspensions. Miconazole and fluconazole are commonly prescribed. Treatment typically lasts 7-14 days.
Vulvovaginal Candidiasis usually responds well to topical antifungal creams or suppositories containing agents like miconazole, clotrimazole or fluconazole. Duration of treatment ranges from 3-7 days depending on the product used. For recurrent infections, longer maintenance therapy with oral fluconazole may be recommended.
Systemic antifungal pills are used for candidiasis that has spread beyond superficial, localized sites. Azoles like fluconazole and newer antifungals like voriconazole are commonly prescribed depending on species identification and susceptibility testing. IV antifungals may be necessary for severe infections in hospitalized patients.
Comprehensive management also involves identifying and addressing predisposing factors to prevent recurrences. Lifestyle changes like a balanced diet, stress management and prompt treatment of underlying conditions can help. With prompt treatment and control of risk factors, the prognosis for Candida infections is usually good. However, systemic and resistant forms still pose therapeutic challenges.
Preventing the Spread of Candidiasis
While Candida naturally lives on and in the human body, it is important to practice good hygiene to prevent its overgrowth and spread to other body sites or individuals:
– Keep oral, genital and skin areas clean and dry.
– Wear loose, breathable cotton underwear and clothes.
– Avoid sharing personal care items that may transfer yeast like towels, clothing and toothbrushes.
– Practice good hand washing, especially before and after using the bathroom.
– See a healthcare provider promptly if symptoms develop for diagnosis and treatment.
– Use condoms during sexual intercourse if an active infection is present.
– Control underlying health issues and work with your provider to prevent recurrences.
In summary, candidiasis is a common fungal infection caused by the yeast Candida. While not usually serious, it can significantly impact quality of life and recurrent forms pose therapeutic challenges. By understanding risks factors, symptoms and preventive measures, individuals can work with their providers to promptly diagnose and manage candidiasis. With treatment and control of underlying conditions, prognosis is usually good.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it